1940s
Department of Medicine founded
The Department of Medicine was established in 1948, two years after the School of Medicine opened in 1946.
Divisions founded
1950s
Divisions founded
Seattle VA
Our affiliation with the VA Puget Sound Healthcare System started in 1951. This still-thriving partnership continues to provide invaluable teaching and research opportunities for the department and the School of Medicine.
Western Association of Physicians
In 1955, Department Chair Dr. Robert Williams, along with five colleagues including Dr. Clement Finch (Hematology Division Head), founded the Western Association of Physicians. The society has grown to several hundred members, including many distinguished academicians from diverse areas of medicine.

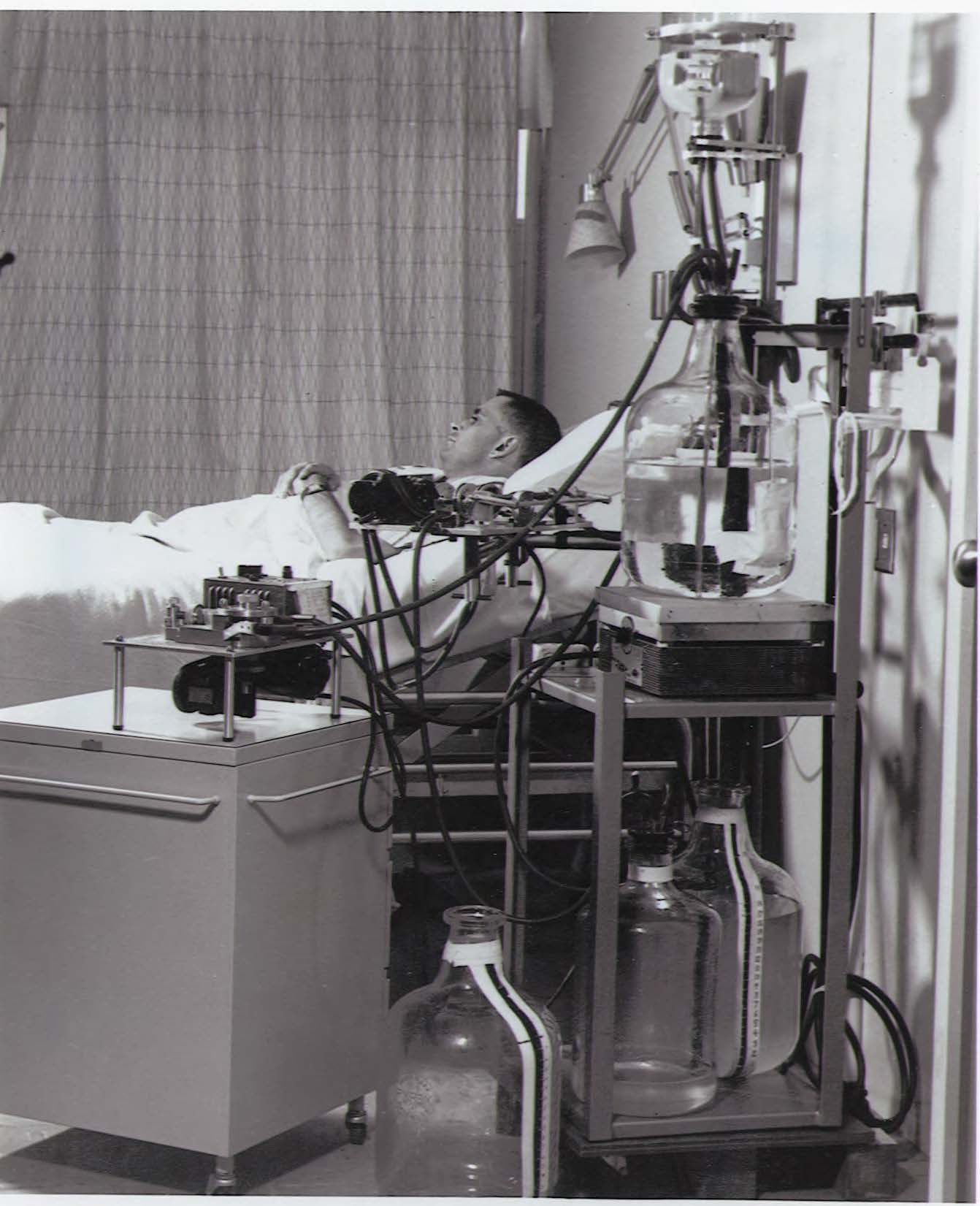
Polio Respiratory Center
One of the ten regional United States Polio Respiratory Centers was established to treat and study the physiology of severely paralyzed patients.
The respiratory centers were the precursors of modern intensive care units.
Internal Medicine Residency Program
In 1957, the Department of Medicine Internal Medicine Residency program began.

Pharmacogenomics
In 1957, medical geneticist Dr. Arno Motulsky founded the field of pharmacogenomics, the study of how drug action and metabolism differ among people due to genetic variability.
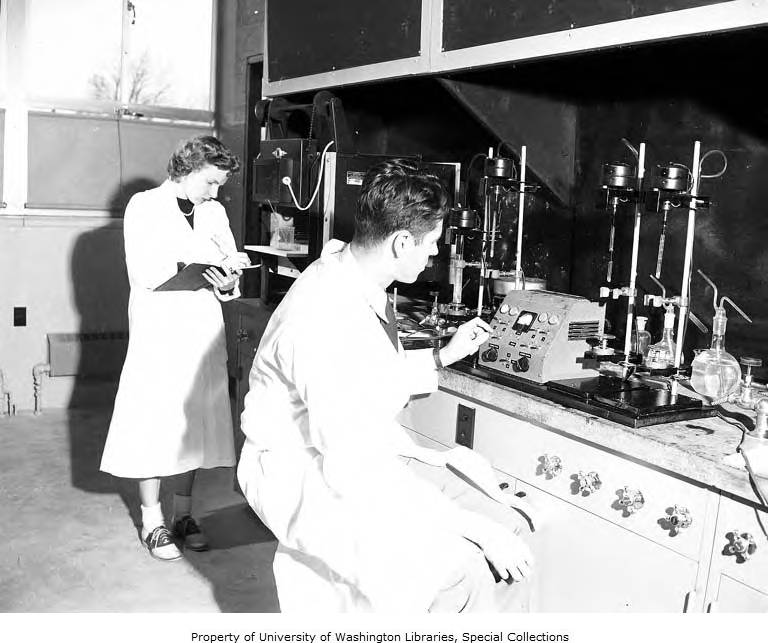
Medical Genetics Clinic
The Medical Genetics Clinic opened at the University Hospital in 1957. Then one of the few genetic disease and counseling clinics in the country, it remains prominent today.
This established the University of Washington as one of only a few medical schools providing training in medical genetics, and as one of the first clinics in the country to provide family counseling for genetic diseases and to employ women in this profession.
University Hospital
The University Hospital (now the University of Washington Medical Center) opened in 1959.
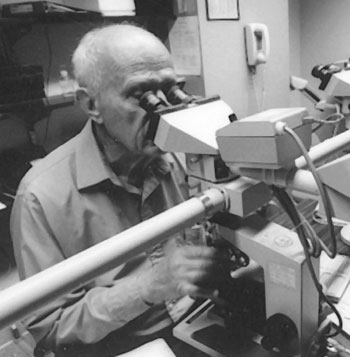
 Anemia
Anemia
Dr. Clement Finch was known as “The Iron Man” for his research on iron metabolization which led to significant advancements in accurately diagnosing and treating anemia.
First documented case of HIV
 In 1959, geneticist Dr. Arno Motulsky collected the first documented human blood sample containing the immunodeficiency virus known as HIV, which causes AIDS.
In 1959, geneticist Dr. Arno Motulsky collected the first documented human blood sample containing the immunodeficiency virus known as HIV, which causes AIDS.
He was collecting samples in the Congo looking for genetic factors that make some people resistant to malaria.
The sample was collected from a Bantu man and kept for decades at the University of Washington and later at the Puget Sound Blood Bank. Motulsky's samples were tested in 1997 using newly available genetic amplification techniques.
Centers founded
- Bloodworks Northwest Research Institute
(Originally King County Central Blood Bank)
1960s
Divisions founded

Clinical Pharmacology
A joint division in the Departments of Medicine and Pharmacology from 1964-1983.
learn more
Respiratory Diseases
Currently the Division of Pulmonary, Critical Care and Sleep Medicine.
learn moreRubin Biopsy Tube
 In the late 1950s and the 1960s, Dr. Cyrus Rubin made engineering advances in gastric and intestinal biopsy leading directly to the accurate diagnosis of celiac disease.
In the late 1950s and the 1960s, Dr. Cyrus Rubin made engineering advances in gastric and intestinal biopsy leading directly to the accurate diagnosis of celiac disease.
Use of the Rubin Tube demonstrated that celiac sprue in children and adults were identical disorders, and his classic 1960 paper established the diagnostic criteria for the disease.

Petersdorf becomes department chair
Dr. Robert G. Petersdorf was appointed department chair in 1964 after serving as chief of medicine at Harborview Medical Center.
Bone Marrow Transplantation
Researchers provided the first demonstration of the feasibility and efficacy of bone marrow transplantation as a curative treatment in human malignancy.
 Harborview Hospital
Harborview Hospital
Harborview Hospital (originally King County Hospital) opened its doors to patients in 1931 and in 1967 the University of Washington was contracted by King County to provide management and operations.
Ambulatory Clinics
Ambulatory internal medicine clinics were initiated at the University's teaching hospitals.
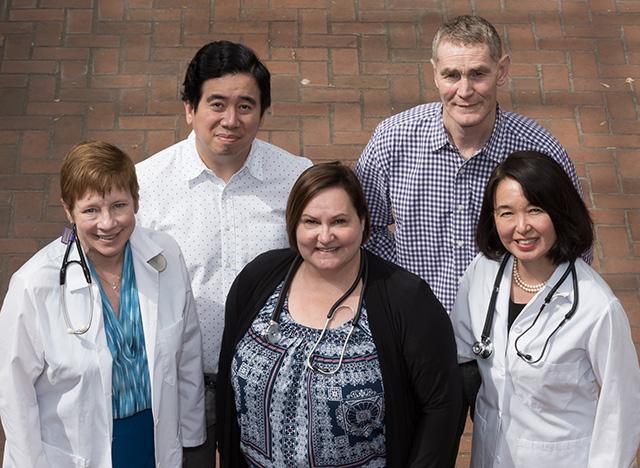
Breaking barriers
 Dr. George Counts was recruited to the University of Washington as a fellow in 1965 and returned in 1975 to become the chief of infectious diseases at Harborview Medical Center.
Dr. George Counts was recruited to the University of Washington as a fellow in 1965 and returned in 1975 to become the chief of infectious diseases at Harborview Medical Center.
He became the first African American professor in the UW School of Medicine in 1985 and was nationally known for his mentorship of minority physicians.
Dermatology Residency Program
The Dermatology Residency Program was created in 1963. It is the only dermatology training program in the five-state WWAMI (Washington, Wyoming, Alaska, Montana, and Idaho) region.
 Pre-hospital care
Pre-hospital care
In the late 1960s, a group of Seattle physicians led by cardiologist Dr. Leonard Cobb recognized the potential for saving the lives of heart attack victims in the pre-hospital setting.
 Scribner Shunt
Scribner Shunt
In 1960, Dr. Belding Scribner and his colleagues developed a blood access device for hemodialysis called the Scribner Shunt, providing a lifeline for patients with kidney failure.
First outpatient dialysis center
Scribner subsequently founded the first outpatient dialysis treatment center in 1962 – the Seattle Artificial Kidney Center – making Seattle an international center for advances in kidney disease. It was later renamed Northwest Kidney Centers.
The first dialysis unit was only big enough for nine patients. Their Admissions and Policy Committee (better known as the “Life and Death Committee”) was an anonymous lay committee responsible for the selection of patients to be treated by the center. This triage was a major step in the development of biomedical ethics.

Odland Bodies

In 1962, Dr. George Odland first described the lamellar granule of the epidermis (Odland body).
This heralded a tradition of scholarly contributions to the understanding of the structure and function of the skin.
Bruce Protocol
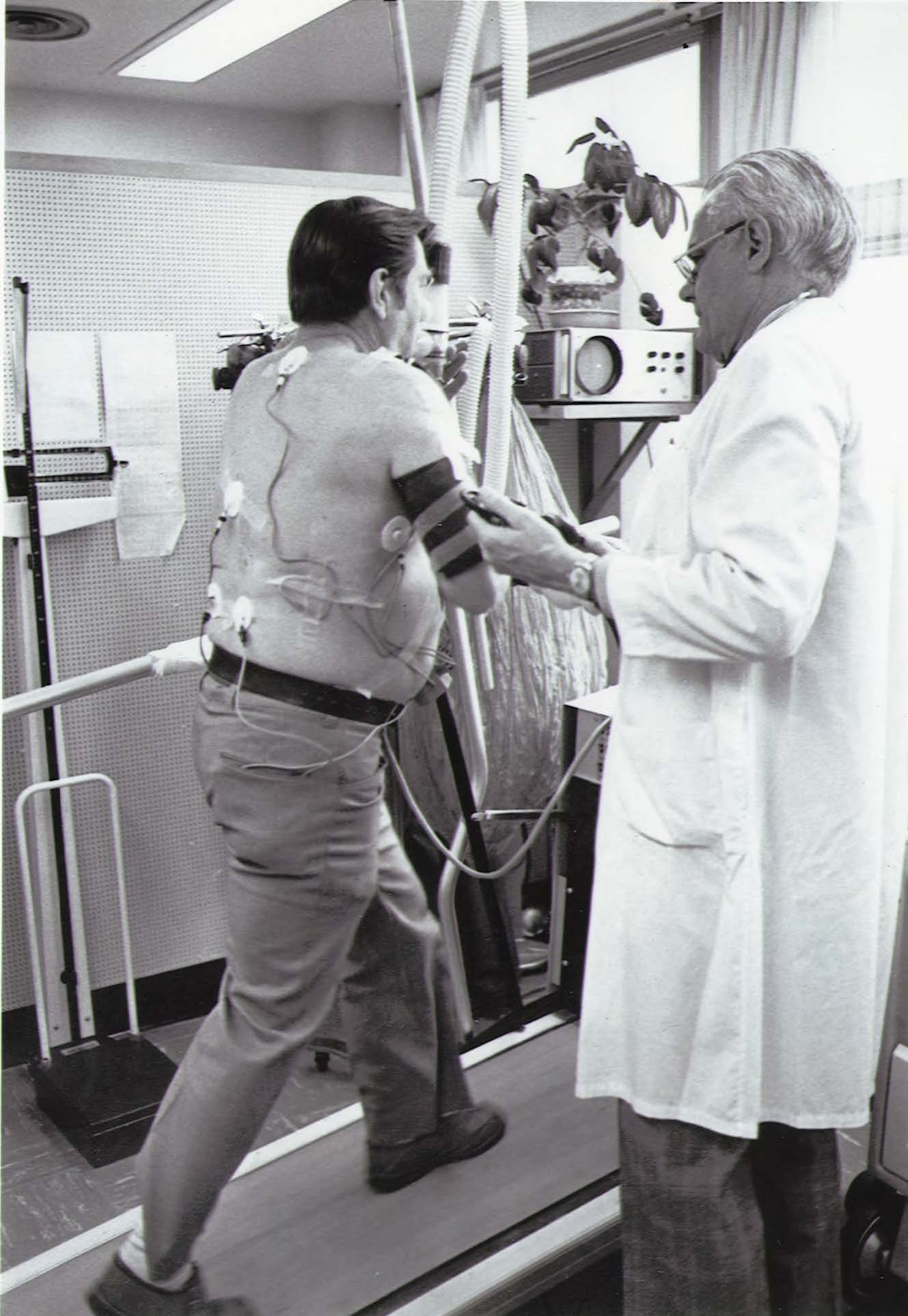 Building on his continued research on the single-stage test, particularly as a predictor of the success of surgery for valvular or congenital heart disease, Dr. Robert Bruce developed the multistage test, consisting of several stages of progressively greater workloads.
Building on his continued research on the single-stage test, particularly as a predictor of the success of surgery for valvular or congenital heart disease, Dr. Robert Bruce developed the multistage test, consisting of several stages of progressively greater workloads.
It was this multistage test, a description of which was first published in 1963, that became known as the Bruce Protocol.
Gut Course
Since its inception in 1968, “The Gut Course,” taught by faculty in the Division of Gastroenterology, has consistently been the highest rated course in the medical school by the students.
Peritoneal dialysis
 A pioneer of peritoneal dialysis, Dr. Henry Tenckhoff was known for developing the first successful indwelling peritoneal dialysis catheter in 1968 which came to be called the Tenckhoff catheter. It remains the most widely used catheter to date.
A pioneer of peritoneal dialysis, Dr. Henry Tenckhoff was known for developing the first successful indwelling peritoneal dialysis catheter in 1968 which came to be called the Tenckhoff catheter. It remains the most widely used catheter to date.
In 1969, he developed the prototype automated home peritoneal dialysis delivery system using a large stainless-steel tank, followed in 1972 by the first automatic peritoneal dialysis system using reverse osmosis to sterilize the dialysate.
Kirby Bauer test
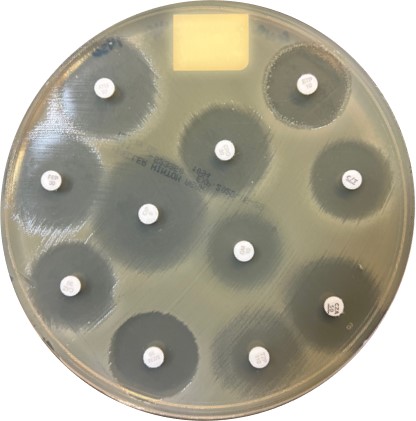 Standardized procedures were developed for testing antibiotic susceptibility using a disk diffusion method.
Standardized procedures were developed for testing antibiotic susceptibility using a disk diffusion method.
The Kirby-Bauer method was named for its creators from the Department of Medicine, Drs. William Kirby and Alfred Bauer (along with Drs. John Sherris and Marvin Turck).
These standards were adopted by the FDA, became accepted worldwide, and led to extensive assessment of the efficacy and clinical utility of many early antimicrobials.
White blood cells kill bacteria
The natural mechanisms by which certain white blood cells (phagocytes) engulf and destroy harmful bacteria – by producing an enzyme called myeloperoxidase – were discovered, changing science’s understanding of the body’s natural defense mechanisms in fighting infections.
This led to new approaches to treating disease when these natural mechanisms are impaired by using therapies to bolster white blood cells.
Ejection fraction
Studies by Drs. J. Ward Kennedy and Harold Dodge helped identify the left ventricle’s “ejection fraction,” a critical measure of cardiac vitality. The ejection fraction is still used widely to diagnose heart disease and to rate damage from heart attacks.
Centers founded
- General Clinical Research Center
1970s

Awards created
Divisions founded
 Medic One
Medic One
The first Medic One call occurred on March 7, 1970, with the patient discharged in good condition after being resuscitated from cardiac arrest.
Seattle Heart Watch
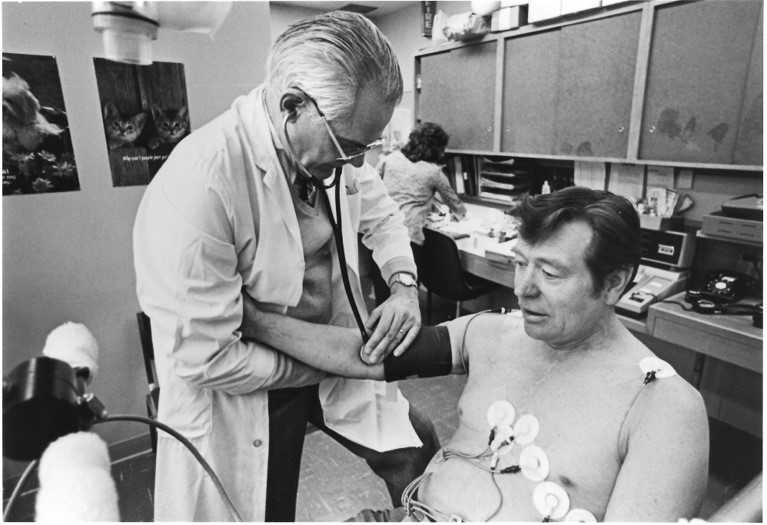 The Seattle Heart Watch program was initiated in 1971 to assess the clinical feasibility of using the treadmill protocol (the Bruce test) in multiple settings.
The Seattle Heart Watch program was initiated in 1971 to assess the clinical feasibility of using the treadmill protocol (the Bruce test) in multiple settings.
It tested the feasibility, utility, and reproducibility of results of symptom-limited exercise testing in ambulatory cardiac patients and healthy subjects.
A database of more than 10,000 individuals was developed over the next 10 years. The duration of exercise became the principal measurement for the estimation of what Bruce termed “functional aerobic impairment.”
Pioneer Square Clinic
The Pioneer Square Clinic was founded in 1971 to provide free healthcare to low-income people and those experiencing homelessness in downtown Seattle
ERCP
Investigators developed ERCP (endoscopic retrograde cholilangiopancreatography) procedures at University Hospital.
ERCP combines X-ray and the use of an endoscope to diagnose and treat problems in the liver, gallbladder, bile ducts, and pancreas.
Familial combined hyperlipidemia
Researchers investigated the genetic basis of hyperlipidemia in coronary heart disease and described a new entity: familial combined hyperlipidemia.
Geriatrics research
An interdepartmental gerontology research center program was established at the University of Washington.
Close interdepartmental collaboration resulted in successful competition and the award of one of the first Geriatric Research, Education, and Clinical Centers (GRECC) to the Seattle and American Lake VA Medical Centers, and the establishment of the Institute on Aging at the University of Washington.
ADA Deficiency
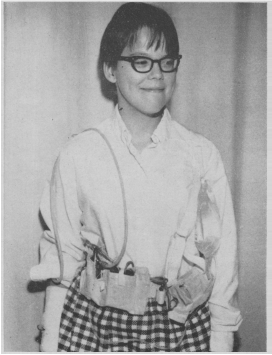
 The first immunodeficiency disease, adenosine deaminase deficiency (ADA), was discovered in 1972 by Dr. Eloise Giblett.
The first immunodeficiency disease, adenosine deaminase deficiency (ADA), was discovered in 1972 by Dr. Eloise Giblett.
Giblet also identified and characterized numerous blood group antigens, including the “Elo” antigen, named after her. Her work paved the way for safer, more effective and more equitable red blood cell transfusions.
Hemophilia
In 1974, one of the first comprehensive regional hemophilia care programs – a world-renowned clinical and research bleeding disorder program – was created to serve patients in the Pacific Northwest.
Asymptomatic gonorrhea study
The asymptomatic gonorrhea study in 1974 revolutionized gonorrhea control and prevention by demonstrating the importance of testing and treating male partners, regardless of symptoms.
Bone marrow transplants
The successful use of autologous bone marrow transplantation was described in 1978; this therapy is now used in more than 30,000 patients annually.
One of the first successful unrelated-donor bone marrow transplants occurred in 1979, leading to a federal law establishing the first-of-its-kind National Marrow Donor Program in 1986.
From Ebola to AIDS
Dr. Peter Piot, a fellow at the University of Washington in the 1970s, co-discovered the Ebola virus in 1976 and went on to work on Project SIDA in Zaire, considered the first international project on AIDS in Africa and providing the first understanding of HIV infection in Africa. He later helped found the United Nations Program on HIV/AIDS.
 Occupational and Environmental Medicine Residency Program
Occupational and Environmental Medicine Residency Program
Established in 1977, the Occupational and Environmental Medicine training program at the University of Washington is one of the longest-standing programs of its kind in the United States.
Chemoradiation
The use of concurrent chemotherapy and radiation was introduced for limited small cell lung cancer and stage 3 non-small cell lung cancer.
Thalassemia
Molecular studies of thalassemia demonstrated many different mutations. Thalessemias were the first human disorders to be delineated at the DNA level.
Acute respiratory distress syndrome
Creation of one of the largest clinical databases of ARDS patients in the world allowed progress in understanding the clinical risk factors that precede ARDS, as well as measurement of disability in survivors and identification of a decline in mortality.
Regional medical education
In response to a critical shortage of physicians, especially those practicing in rural areas, the WAMI (Washington, Alaska, Montana, and Idaho) program was initiated in the early 1970s as the regional medical education network of the University of Washington School of Medicine. Wyoming would join in 1996.
Today, this regional medical education program known as WWAMI (an acronym representing the states it serves) is heralded as one of the most innovative medical education and training programs in the country.

Groundbreaking residency training program
A groundbreaking residency training program in Primary Care Internal Medicine was established in 1977 with two primary care tracks (one based entirely in Seattle and one with a year in Boise, Idaho).
There are now two Internal Medicine Residency Programs, one in Seattle and one in Boise.
STD prevention training
The STD & AIDS Research Training program was established in 1974 and has trained nearly 250 pre- and postdoctoral trainees.
A Centers for Disease Control-funded regional training center was created in 1979 to instruct healthcare practitioners in the management of sexually transmitted diseases. The center continues to operate.
Cardiac imaging
Researchers were among the first to introduce thallium myocardial imaging, which became the mainstay of nuclear cardiology. Thallium myocardial imaging accurately provides information about the distribution of coronary blood flow to the cardiac muscle.
Artificial gut
Researchers created the artificial gut, which became known as home parenteral nutrition. The procedure provides full nutritional support at home using the intravenous route and is used on patients whose bowel function is lost due to chronic bowel diseases.
Fred Hutchinson Cancer Research Center

An affiliation with the Fred Hutchinson Cancer Research Center, which opened its doors in 1975, has continued to deepen and flourish into a prolific and integrated partnership.
Modern primary care
Drs. Thomas Inui and James Logerfo helped establish the field of clinically oriented health services research.
With colleagues around the country, they formulated the concept of modern primary care and founded the Society of General Internal Medicine in 1978.
Inui started the first primary care clinic in the entire VA system. He went on to become the first head of the Division of General Internal Medicine.
Senior care
The SeniorCare Program – a continuum of geriatric health care to serve as a learning laboratory for medical students, residents, and fellows – was initiated at Harborview Medical Center and continues today.
Hickman Catheter
 In 1979, Dr. Robert Hickman created the Hickman catheter, a lifesaving device that revolutionized care for cancer patients and transformed doctors’ ability to access a patient’s bloodstream.
In 1979, Dr. Robert Hickman created the Hickman catheter, a lifesaving device that revolutionized care for cancer patients and transformed doctors’ ability to access a patient’s bloodstream.
The device is still used worldwide to deliver IV nutrition, draw blood, and deliver chemotherapy.
Dementia
Neurologist Dr. Thomas Bird was studying degenerative neurologic diseases that led to the discovery of one of the first Alzheimer’s genes. He opened the Adult Neurogenetics Clinic in 1974.
Centers founded
- Cardiovascular Research & Training Center
- Center for Research in Reproduction & Contraception
- Diabetes Research Center
- Virology Research Clinic
1980s

Awards created

Fialkow becomes department chair
In 1980, Dr. Philip J. Fialkow became the third chair of the Department of Medicine. He had served as chief of medicine at the Seattle VA since 1974.
Effectiveness of defibrillation
 Research in the 1980s provided the first demonstration of the effectiveness of defibrillation performed by paramedics.
Research in the 1980s provided the first demonstration of the effectiveness of defibrillation performed by paramedics.
Faculty worked closely with industry to help design effective and smaller implantable cardiac defibrillators. This work culminated in the development of defibrillators that can be placed into the heart through catheter techniques without the need for cardiac surgery.
Antiviral therapy
Researchers demonstrated the effectiveness of the world’s first antiviral therapy (acyclovir) for the treatment of genital herpes in the early 1980s, paving the way for antiviral therapy for HIV, cytomegalovirus, hepatitis B, hepatitis C and influenza.
Streptokinase
In the 1980s, researchers led a study of an enzyme, streptokinase, later found to be safe and effective in breaking up blood clots that might cause repeat heart attacks.
Streptokinase has since been used worldwide, especially in situations where a catheter is not available for angioplasty.
Cardiac Transplantation
A state-of-the-art program in cardiac transplantation was developed in the 1980s.
Southeast Asian Refugee Clinic

The Southeast Asian Refugee Clinic, now called the International Medicine Clinic, was established in 1984 at Harborview Medical Center.
Today, the clinic, which has achieved a national reputation for developing resources to improve the care of refugee populations, has more than 12,000 visits a year and provides tailored primary and mental health care to refugees, asylum seekers, trafficked persons, and immigrants.
 Joseph Goldstein receives Nobel Prize
Joseph Goldstein receives Nobel Prize
Dr. Joseph Goldstein, a molecular geneticist and former trainee of Dr. Arno Motulsky, received the Nobel Prize in Physiology or Medicine in 1985 for elucidation of the process of cholesterol metabolism in the human body.
Research-focused fellowship programs
The VA Health Services Research and Development fellowship program and the NIH National Resources Service Administration fellowship program were initiated. Patterned after the Robert Wood Johnson Clinical Scholars Program, the VA and NRSA programs draw from a nationwide pool of highly qualified trainees, more than 80% of whom pursue academic careers.
Northwest Geriatrics Education Center
The Northwest Geriatrics Education Center was established in 1985 as part of a network of programs established to strengthen interdisciplinary training of health professionals in the health concerns of older adults.
Rheumatoid arthritis
Faculty discovered the high prevalence of rheumatoid arthritis among Native Americans of the Yakima tribe, known to have the highest prevalence of the disease in the world.
Self-association of lgG-rheumatoid factors was discovered in patients with rheumatoid arthritis. These unique immune complexes contribute to the joint inflammation of rheumatoid arthritis.
A case-controlled study in the 1980s found that the use of oral contraceptives decreases the incidence of rheumatoid arthritis in women.
One of the first placebo-controlled studies on the benefit of treating rheumatoid arthritis with methotrexate was conducted by researchers in 1980. Currently, methotrexate is among the most used drugs for the treatment of rheumatoid arthritis.
Lipid-lowering therapy for heart disease
Researchers led one of the first clinical studies to demonstrate a reduction in coronary artery disease severity with lipid-lowering treatment with statins.
Endoscopic instruments 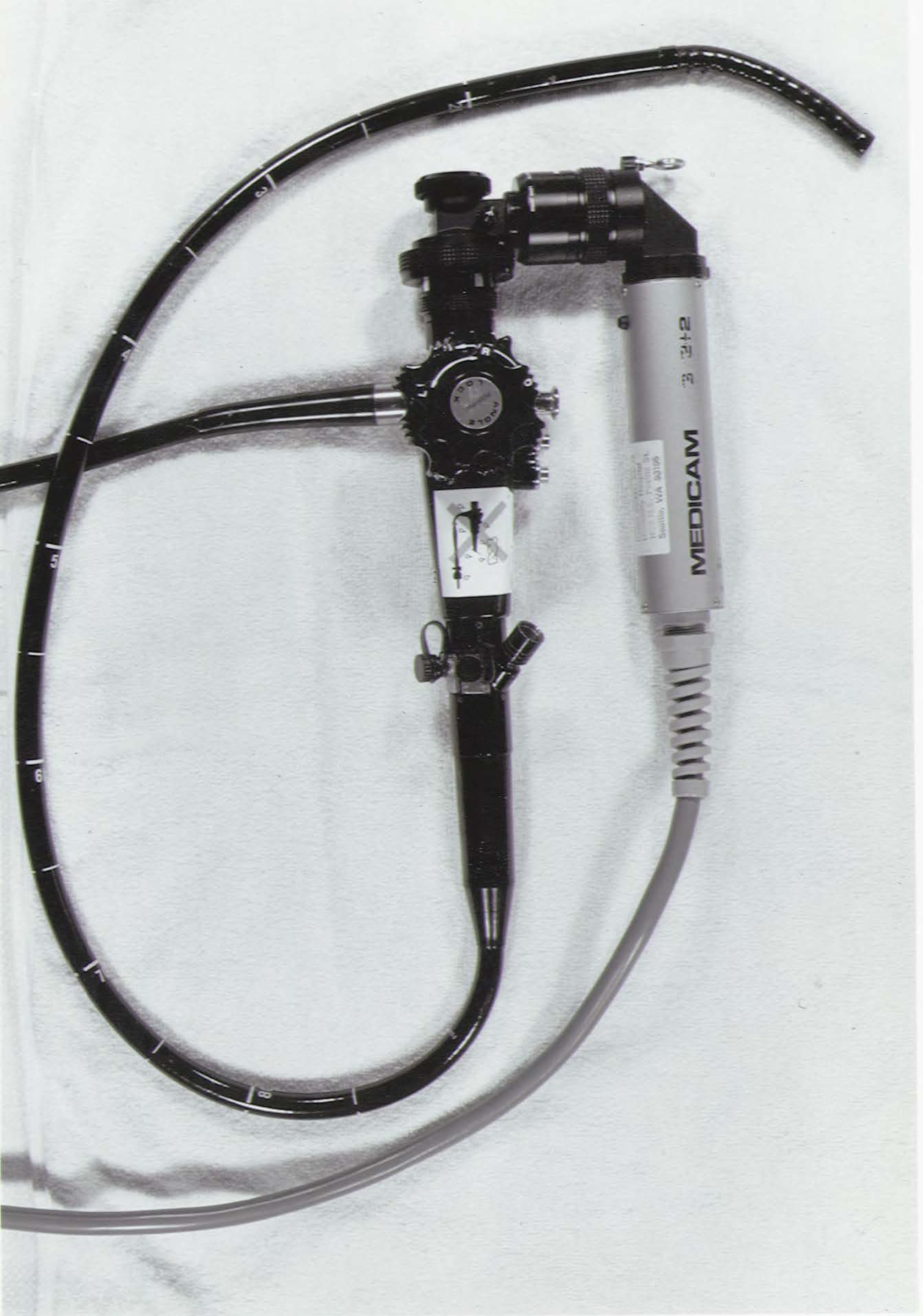
A variety of endoscopic instruments and accessories were designed and constructed, including laser therapy for upper gastrointestinal bleeding and electro-coagulation instruments for curtailing gastrointestinal bleeding.
Devices such as the heater probe and the BICAP probe were developed and are now used internationally in clinical medicine.
Japanese American Community Diabetes Study
The pivotal Japanese American Community Diabetes Study started in Seattle in 1983 and continued for 18 years with over 600 participants. The study recognized the high incidence of type 2 diabetes in the Asian American community.
Cystic Fibrosis
Investigators began the first cystic fibrosis program for adults in the Pacific Northwest in 1989. The Cystic Fibrosis Research Development Program has developed into a leading cystic fibrosis clinical studies center.
 HIV/AIDS
HIV/AIDS
In 1981, the Centers for Disease Control reported the first cases of what would become known as HIV/AIDS. Harborview Medical Center became one of the first hospitals in the country to open a specialty clinic for HIV/AIDS patients.
Small at first, this clinic was the basis for the larger Madison Clinic, which opened in 1985 and continues today.
Centers founded
- Cardiovascular Health Research Unit
- Center for AIDS and STD
- Center for AIDS Research
- Nutrition Obesity Research Center
- UW Positive Research
(Originally AIDS Clinical Trial Unit) - VA Research Centers
1990s

Awards created
- Fialkow Scholar Award
- WWAMI Excellence in Teaching Awards

The spotlight title goes here
The spotlight subtitle goes here.
Divisions founded

Ramsey becomes department chair
In 1990, Dr. Paul G. Ramsey was appointed as chair of the department after serving for 18 months as acting chair. He went on to become dean of the School of Medicine in 1997.
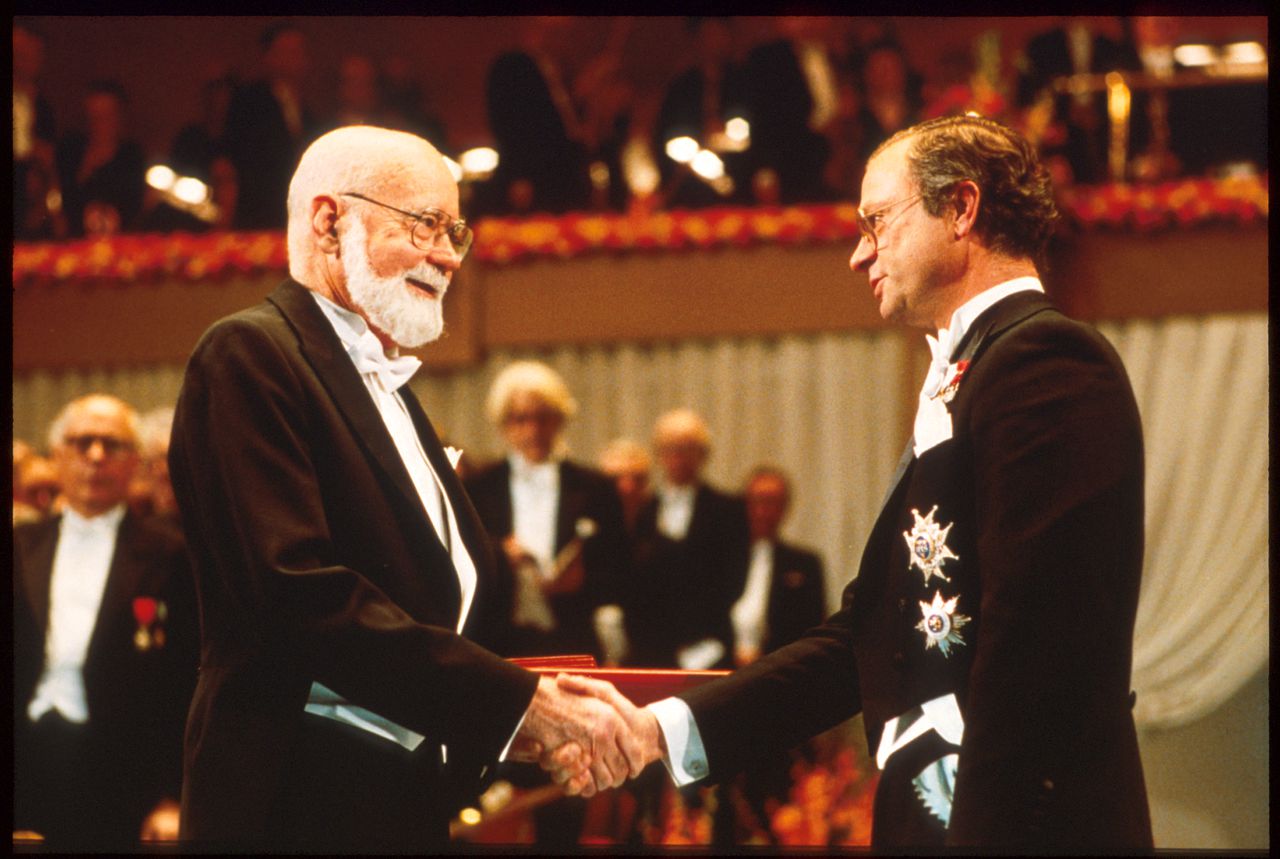 E. Donnall Thomas receives Nobel Prize
E. Donnall Thomas receives Nobel Prize
The Nobel Prize in Medicine was awarded to Dr. E. Donnall Thomas in 1990. Thomas was known as the father of bone marrow transplantation, for his work related to the development of bone marrow grafting techniques.
Gene Therapy
The Markey Molecular Medicine Center was founded in 1990 to recruit faculty in genomics, developmental genetics, and gene therapy.
The University of Washington Gene Therapy Program was established, and a gene therapy laboratory designed to transfer gene therapy research to clinical applications was established in the Clinical Research Center.
Dr. George Stamatoyannopoulos founded the American Society of Gene and Cell Therapy in 1996, now the pre-eminent scientific forum for a field numbering thousands of scientists spanning academia and biotechnology. He was head of the Division of Medical Genetics from 1989-2005.
Diabetes Care Center
The University of Washington Diabetes Care Center opened to patients in 1991 and was a showcase for the institution.
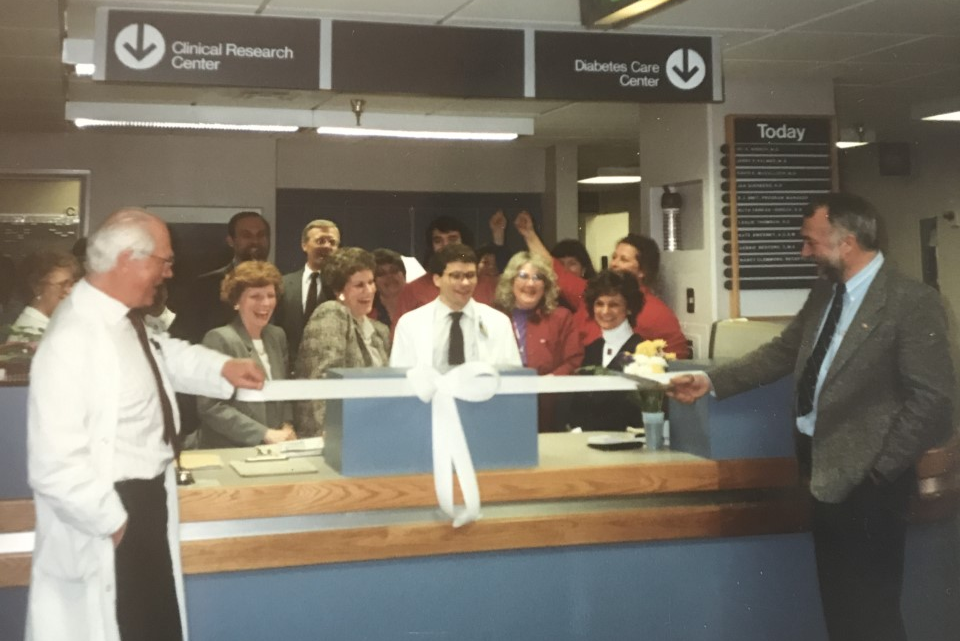
It has served as the springboard for many additional diabetes initiatives including the Diabetes Care Center in 1991, the Diabetes and Obesity Center of Excellence in 2008, the Diabetes Institute in 2019, and the Latinx Diabetes clinic in 2020.
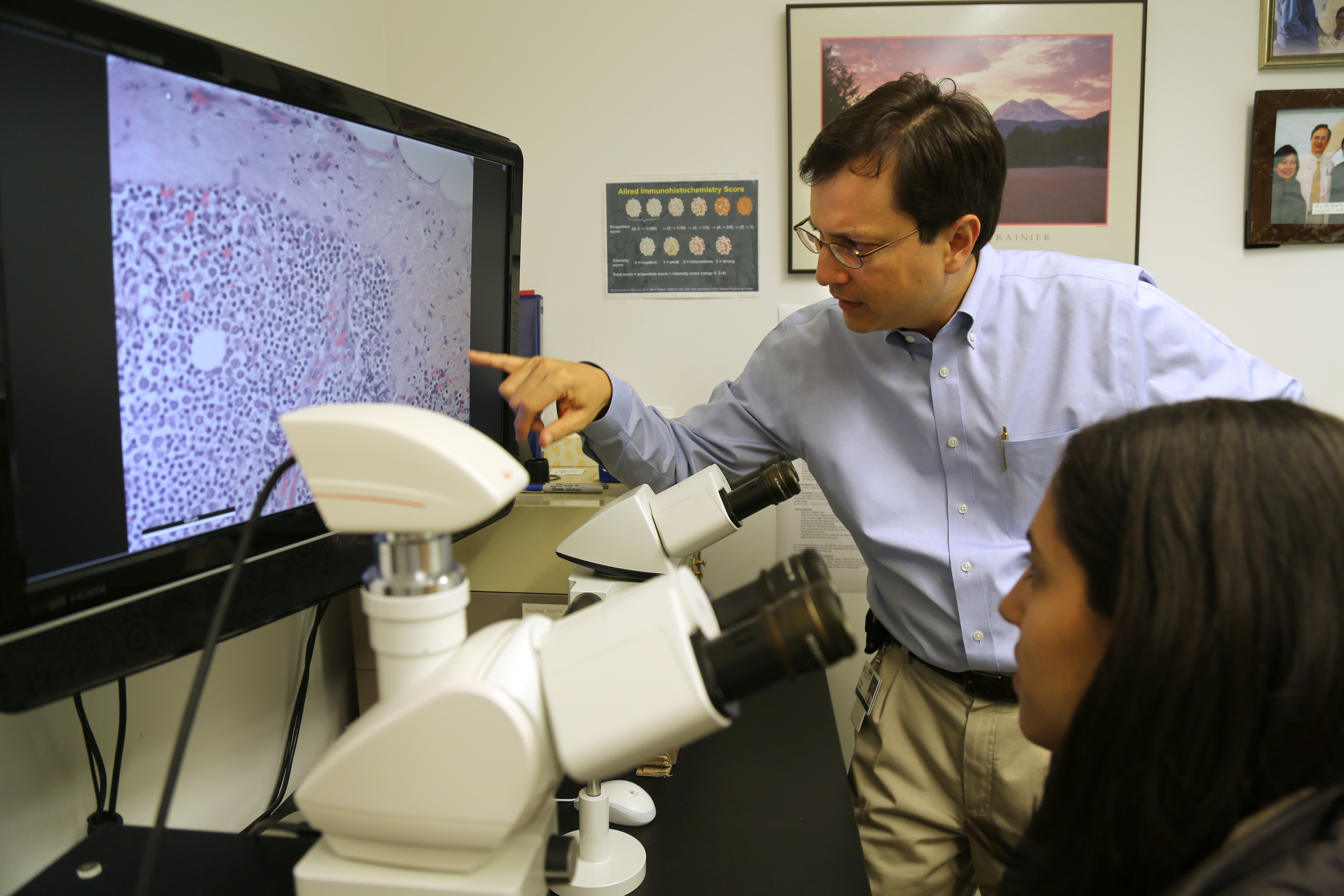
Pancreatic cancer
 In 1994, Dr. Teresa Brentnall and colleagues developed a multidisciplinary surveillance program – the first of its kind in the world – for the early detection of pancreatic cancer and its precursors in patients with a familial predisposition for the diseases.
In 1994, Dr. Teresa Brentnall and colleagues developed a multidisciplinary surveillance program – the first of its kind in the world – for the early detection of pancreatic cancer and its precursors in patients with a familial predisposition for the diseases.
Discovery of palladin
In 2006, they discovered that a mutated gene called palladin can cause pancreatic cancer in families.
Lung transplants
The lung transplant program at UW Medical Center was established in 1991 and is the only lung transplant program in the Pacific Northwest. The team has performed over 1000 lung transplants.
Non-Hodgkin’s Lymphoma
Targeted radioimmunotherapy was developed as a potentially curative treatment for non-Hodgkin's lymphoma.
Glutamic acid decarboxylase
The human islet antigen, glutamic acid decarboxylase (GAD), was cloned, and recombinant GAD was used for immunoassays to predict the development of insulin-dependent diabetes in humans. This assay has now been standardized and is used worldwide.
Fluorescent microsphere technology
The fluorescent microsphere technology was developed. It defined a completely new explanation for regional differences in pulmonary blood flow distribution.

Werner Syndrome
The gene for Werner Syndrome (premature aging) was cloned and identified as a DNA-unwinding enzyme (helicase).
Barrett’s Esophagus
A biopsy protocol that involves high-density biopsy sampling every 1-2 cm of the Barrett’s esophagus segment (the Seattle protocol) was developed and considered to be the optimal method for detecting early cancers in patients with high-grade dysplasia.
Color vision
The molecular basis of color vision was elucidated. Demonstration of the differences in color perception due to a simple polymorphism in the visual pigment genes resulted in the establishment of a new field of molecular psychology.
Mini-transplant
In 1997, Dr. Rainer Storb and colleagues developed a radically different approach to bone marrow transplantation.
It offered hope for older or otherwise medically unfit blood cancer patients whose bodies could not withstand the rigors of a conventional transplant.
This treatment, called the non-myeloablative stem cell transplant, or "mini-transplant," does not wipe out bone marrow and involves minimal radiation. Studies have shown that patients are as likely to survive following a reduced-intensity transplant as the conventional transplant.
Medical Genetics Residency Program
Dr. Philip Fialkow, former chair of the department and dean of the School of Medicine, started the Medical Genetics fellowship in 1963, which evolved into the residency program in 1997, complemented by a T32 postdoctoral training program.
In 2017, the combined Pediatric-Medical Genetics Residency Program was established.
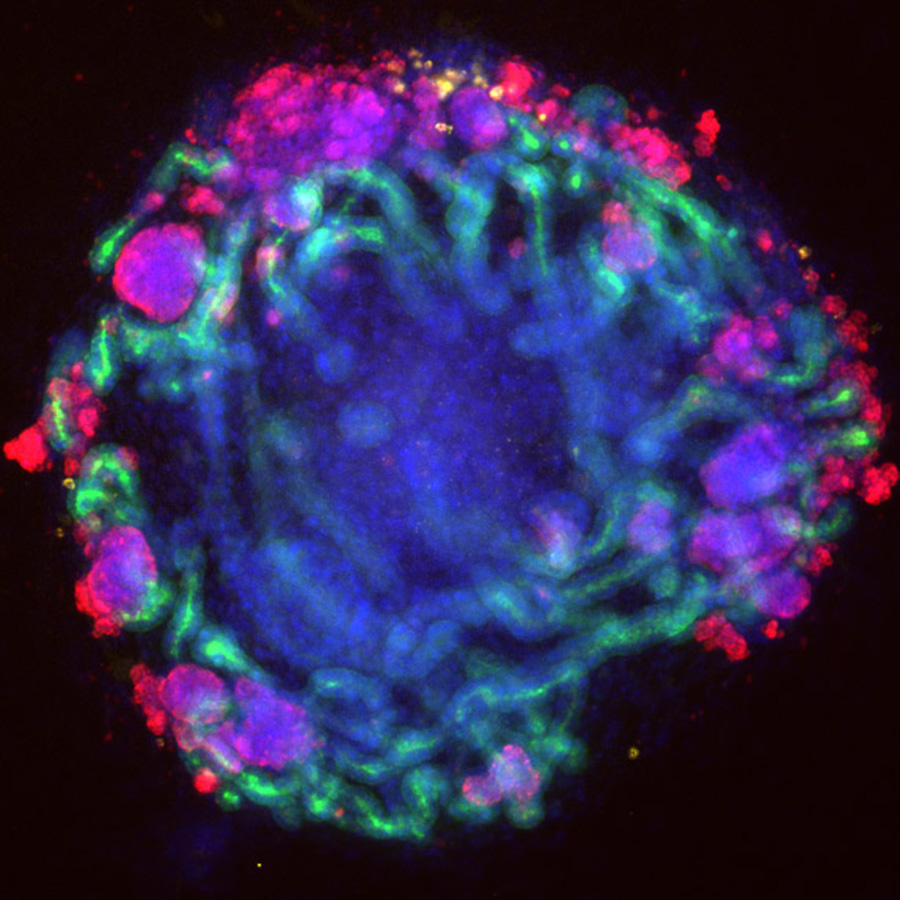
Adoptive immunotherapy
In a landmark study, billions of cytotoxic CDS+ T-lymphocyte clones rendered reactive against cytomegalovirus were infused into marrow transplant recipients and were shown to persist, function, and prevent potentially fatal infection.
Seattle Cancer Care Alliance
 In 1998, Fred Hutch, Seattle Children’s and UW Medicine joined forces to form the Seattle Cancer Care Alliance to lead the world in translating scientific discovery into the prevention, diagnosis, treatment and cure of cancer.
In 1998, Fred Hutch, Seattle Children’s and UW Medicine joined forces to form the Seattle Cancer Care Alliance to lead the world in translating scientific discovery into the prevention, diagnosis, treatment and cure of cancer.

Bremner becomes department chair
In 1998, Dr. William Bremner, vice chair of the department since 1987, became the fifth chair of the Department of Medicine, a position he would hold for the next 20 years.
Centers founded
- Cancer Vaccine Institute
(Originally Tumor Vaccine Group)
2000s

Leland Hartwell receives Nobel Prize
 The Nobel Prize was awarded to Dr. Leland Hartwell in 2001 for discoveries of protein molecules that control the division of cells.
The Nobel Prize was awarded to Dr. Leland Hartwell in 2001 for discoveries of protein molecules that control the division of cells.
Through studies of yeast in 1971, Hartwell was able to identify hundreds of genes that govern cell division. He also showed that the cell cycle comes to a halt if the cell’s DNA is damaged.
Colleges System
Dr. Erika Goldstein was founding director of the School of Medicine Colleges System. Established in 2001, this is a four-year integrated learning community focused on a deepening understanding of fundamental clinical skills and professionalism linked to a robust mentoring program.
Molecular Medicine Training Program
In 2005, the Molecular Medicine Training Program was established to link basic science and clinical investigation.
Women's Empowerment Cancer Advocacy Network
The Women’s Empowerment Cancer Advocacy Network was founded in 2003 by Dr. Julie Gralow to support patient advocates in low- and middle-resource countries. The network is still going strong today.

Cancer Consortium
In 2002, the University of Washington joined with Fred Hutchinson and Seattle Children’s to form the Cancer Consortium, the only National Cancer Institute (NCI) designated comprehensive Cancer Center in Washington state. The Seattle Cancer Care Alliance joined the consortium in 2008.
Project ECHO
 Launched in 2009 as one of only two in the nation, UW Project ECHO (Extension for Community Healthcare Outcomes) is a revolutionary guided-practice model that reduces health disparities in underserved and remote areas of the state, nation and world.
Launched in 2009 as one of only two in the nation, UW Project ECHO (Extension for Community Healthcare Outcomes) is a revolutionary guided-practice model that reduces health disparities in underserved and remote areas of the state, nation and world.
Lung Cancer Early Detection
Unique to the region, the Lung Cancer Early Detection and Prevention Clinic opened in 2007 to provide risk assessment and screening for those who have been exposed to smoke or diagnosed with lung nodules.
Institute of Translational Health Sciences

The Institute of Translational Health Sciences was established in 2007, one of more than 50 Clinical and Translational Science Award sites nationwide working to change how biomedical research and training is performed.
Regional Native American Community Networks Program
The Regional Native American Community Networks Program was established in 2006 to address cancer-related disparities among American Indians and Alaska Natives in the Pacific Northwest and Northern Plains states.
Melanoma
The first successful use of a human patient's cloned infection-fighting T cells as the sole therapy to put an advanced solid-tumor cancer (Melanoma) into long-term remission was described in 2008.
Researchers were later instrumental in the clinical trials of two checkpoint inhibitors, anti-PD-1 and anti-PD-L1, to treat melanoma.
This research helped to develop two FDA-approved checkpoint inhibitor drugs — pembrolizumab and nivolumab — that are now used to treat melanoma, lung cancer, head and neck cancers and other cancers.
Mindfulness-based stress reduction
In 2008, a mindfulness-based stress reduction course started at the Seattle VA to help veterans with post-traumatic stress disorder (PTSD) as part of a first-of-its-kind study to determine the effectiveness of this type of treatment for PTSD.
Heart and aging research
In 2008, the CHARGE (Cohorts for Heart and Aging Research in Genomic Epidemiology) consortium started with 5 U.S. and European cohort studies and soon expanded to 10, to facilitate genome-wide association study meta-analyses and replication opportunities among multiple large and well-phenotyped longitudinal cohort studies.
These cohorts have an extensive collection of genomic data as well as repeated measures of risk factors, subclinical disease indicators, and cardiovascular events on over 50,000 multi-ethnic participants.
Continuous glucose monitoring
In 2008, investigators at the University of Washington reported work in the first randomized controlled trial for continuous glucose monitoring for type 1 diabetes.
These investigators played a pivotal role in the 2010s in developing the first hybrid closed-loop automated insulin delivery systems.
2010s

Awards created
- Chair of Medicine Scholars Award
- C. Scott Smith Community Teacher of the Year Award
- Housestaff Research Mentor Awards
- Hindson Award
- Mentorship awards
- Outstanding Student Awards
- Resident and Intern Excellence in Teaching Awards
- UWMC Chief of Medicine Service Awards
- Violet Zuvela Primary Care IM Scholarship Award
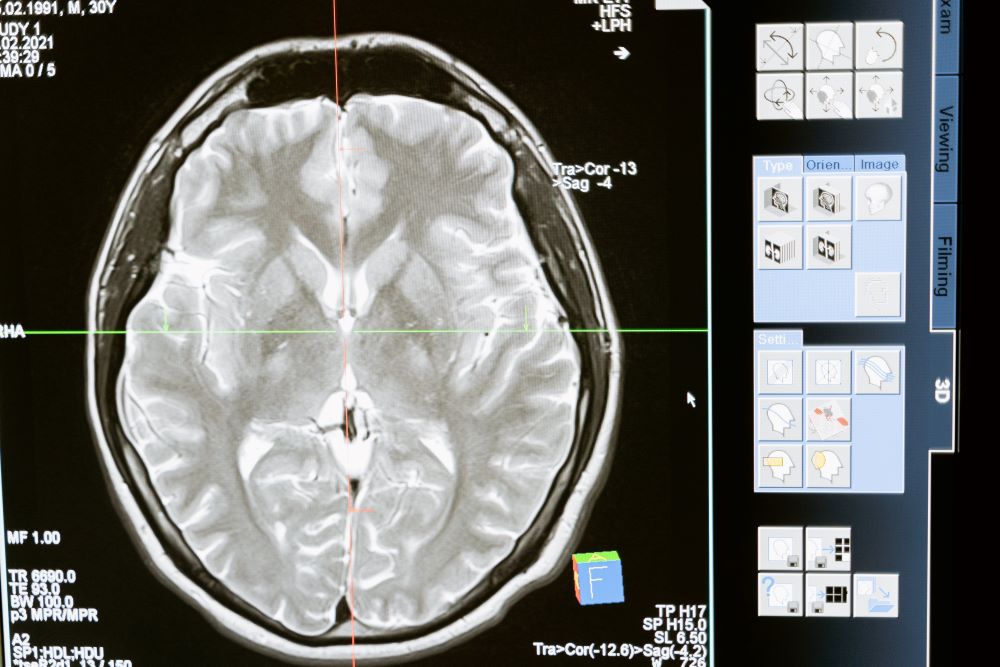
Brain and insulin
Pivotal studies that started in 2010 and continue today demonstrate that the brain, and in particular the hypothalamus, plays a pivotal role in the development of obesity and insulin resistance.
These insights suggest that new therapies targeting neurocircuitry could be fundamental in overcoming the obesity epidemic.
Insulin and memory care
Alzheimer’s disease and other, similar forms of dementia have become one of the most severe socioeconomic and medical burdens impacting modern society.
A research group studying intranasal compounds to treat dementia discovered that insulin delivered high up in the nasal cavity goes to affected areas of the brain with lasting results in improving memory.
AIDS treatment and research
Partners PrEP
In 2011, the landmark Partners PrEP (pre-exposure prophylaxis) study, conducted in Kenya and Uganda, showed that participants who took a daily pill — a mix of tenofovir and emtricitabine — had a 73 percent lower chance of getting infected. The study was one of the first to show protection in heterosexuals.
HIV control and treatment
In 2017, the Department of Medicine led the first known achievement of the UNAIDS goal of 90-90-90 for HIV control and treatment (90% of all people living with HIV will know their HIV status, 90% of all people with diagnosed HIV infection will receive sustained antiretroviral therapy, and 90% of people receiving antiretroviral therapy will have viral suppression.)
HIV testing in immigrant communities
In 2018, the first phase of a community-based participatory research project called Harambee! achieved a more than 50% uptake of HIV testing in local Somali, Ethiopian and Eritrean immigrant communities.
Palliative care
Homeless Palliative Care Outreach Program
The Homeless Palliative Care Outreach Program at Harborview’s Pioneer Square Clinic, launched in 2014, is the first of its kind in the country and one of only a handful in the world.
Certified care
In 2016, UW Medicine became the first healthcare system in the country to achieve certification at all its hospitals from the Joint Commission’s Advanced Certification Program for Palliative Care.
Palliative Care Dialysis Program
A novel palliative care/dialysis program has enrolled over 400 patients since its start in 2017.
Boise IM Residency Program

Boise became the second Internal Medicine Residency Program under the University of Washington umbrella in 2011, with a mission to train superb physicians for Idaho and its neighboring states with a focus on practice in general internal medicine.
85% of program graduates stay in internal medicine, more than 60% stay in Idaho to practice, and 15% practice in neighboring states.
Residency program in Kenya
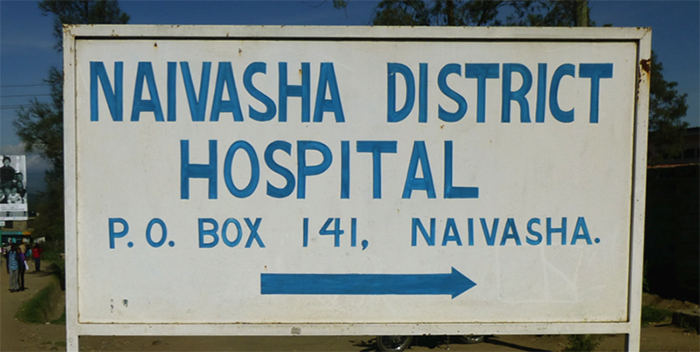 In 2012, a new residency program started at a rural hospital in Kenya – the Naivasha District Hospital – as part of the Clinical Education Partnership Initiative (CEPI).
In 2012, a new residency program started at a rural hospital in Kenya – the Naivasha District Hospital – as part of the Clinical Education Partnership Initiative (CEPI).
Offering a one-month elective in Kenya for residents interested in global health, the program also matches with residents at the University of Nairobi.
Centers of Excellence in Primary Care Education
The VA Puget Sound Healthcare System and the Boise VA were two of five VA medical centers to establish a Center of Excellence in Primary Care Education.
Center of Excellence in Pain Education
In 2012, the NIH Pain Consortium selected the University of Washington as one of the 11 Centers of Excellence in Pain Education to develop pain curricula.
Molecular Medicine and Mechanisms of Diseases PhD Program
The Molecular Medicine and Mechanisms of Diseases PhD Program (M3D) was established in 2014. This is an interdisciplinary and interdepartmental PhD Program designed for students who seek to pursue careers in translational research via PhD training in basic science.
Colorectal Cancer Trial
Launched in 2012 and led nationally by researchers at the Seattle VA, the colorectal cancer trial is the largest VA clinical trial in history.
The study assesses long-term cancer-related mortality and incidence after screening with either colonoscopy or annual fecal immunochemical testing (FIT). Researchers have enrolled over 50,000 Veterans at average risk for colorectal cancer.
VA transplant programs
The Lung Transplant Program was established at the Seattle VA in 2012, one of only two programs nationwide.
In 2016, the Seattle VA Marrow Transplant Unit performed its 1500th hematopoietic stem cell transplant since opening in 1982. The Seattle VA was the first in the country to have a transplant unit. It was founded by former professor Dr. Jack Singer, who served as its director from 1982-1992.
Kidney-on-a-chip
 In 2012, the Kidney Research Institute (KRI) received an award from the National Center for Advancing Translational Sciences to engineer a kidney tissue chip to test drug therapies against diseases without putting actual patients in danger of side effects.
In 2012, the Kidney Research Institute (KRI) received an award from the National Center for Advancing Translational Sciences to engineer a kidney tissue chip to test drug therapies against diseases without putting actual patients in danger of side effects.
In 2019, a rocket transported the chips to the International Space Station. This novel space medicine project was an attempt to understand how microgravity and other factors worsen kidney health.
In 2020, KRI researchers received funding to test the kidney chip’s prospects for making clinical trials more useful.
Adolescent and Young Adult Diabetes Program
The joint University of Washington/Seattle Children’s Adolescent and Young Adult Diabetes Program was established in 2015.
The first of its kind on the West Coast, this program addresses the unique health needs of patients transitioning from pediatric to adult diabetes care, a time when patients are particularly vulnerable and may have gaps in care with long-term, devastating consequences.
Diabetes and cardiovascular disease
The leading cause of death for persons with diabetes is cardiovascular disease. In 2018, a lipoprotein-associated protein, apolipoprotein C3, was described as a biomarker and mediator of cardiovascular disease associated with type 1 diabetes.
Advances in cardiac care
Risk modeling in heart failure
The Seattle Heart Failure Model was developed in 2006 to predict the survival of heart failure. In 2015, the Seattle Proportional Risk Model was developed to determine which heart failure patients were at greatest risk of sudden death, and in 2018, the model was used to predict who would benefit from an implantable cardioverter-defibrillator (ICD).
Subcutaneous ICD
In 2012, the Federal Drug Administration approved the first subcutaneous implantable cardioverter-defibrillator, created by cardiologist Gust Bardy.
MitraClip Therapy
In 2015, the 100th patient was treated with MitraClip, a therapy that offers a significant treatment advance by using a less-invasive and catheter-based approach to repair the mitral valve.
By 2022, 660 patients had been treated with this therapy.
The University of Washington is one of the top five sites providing this unique therapy in the United States.
Transcatheter aortic valve replacement

In 2017 the UW Medicine cardiac team was first-in-the-world to employ intentional cut via catheter to replace a patient’s failed artificial aortic valve.
The minimally invasive transcatheter aortic valve replacement (TAVR) allows patients who are too old or weak for open heart surgery to receive the same life-extending device.
Precision Medicine
Brotman Baty Institute
The Brotman Baty Institute for Precision Medicine was founded in 2017 to foster collaborative work across UW Medicine, Fred Hutchinson Cancer Center and Seattle Children’s and accelerate research and discovery in the field of precision medicine.
Kidney Precision Medicine
In 2017, the University of Washington, with collaborators at the University of Michigan and the Icahn School of Medicine at Mount Sinai, was named the Central Hub of the new Kidney Precision Medicine Project, a national consortium that seeks to redefine acute and chronic kidney diseases in molecular terms and identify novel targeted therapies.
Trans-Omics for Precision Medicine
A research repository was established for the National Heart, Lung, and Blood Institute Trans-Omics for Precision Medicine (TOPMed) program, an effort to identify genetic and other molecular risk factors for heart, lung, blood, and sleep disorders.
Precision Medicine Cohort Sequencing Center
 In 2018, the University of Washington became an All of Us National Precision Medicine Cohort Sequencing Center, gathering data from participants from many backgrounds to create a national medical research resource for improving precision medicine.
In 2018, the University of Washington became an All of Us National Precision Medicine Cohort Sequencing Center, gathering data from participants from many backgrounds to create a national medical research resource for improving precision medicine.
Almost 100,000 highly diverse whole genome sequences are now available through this program, and about 50% of the data is from individuals who identify with racial or ethnic groups that have historically been underrepresented in research.
Precision oncology
In 2022, Fred Hutch received a transformative gift to establish a new precision oncology institute to drive precision oncology discoveries and accelerate the future of cancer research.
Malaria Box
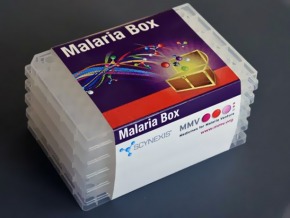 In an unprecedented and successful open-source drug discovery experiment in 2016, the Medicines for Malaria Venture (MMV) distilled over 25,000 active inhibitors (or "killers") of malaria into a group of 400 malaria-killing compounds.
In an unprecedented and successful open-source drug discovery experiment in 2016, the Medicines for Malaria Venture (MMV) distilled over 25,000 active inhibitors (or "killers") of malaria into a group of 400 malaria-killing compounds.
The “Malaria Box” was distributed to researchers around the world, including the University of Washington.
The project was successful in identifying compounds to pursue for antimalarials, as well as compounds to treat other parasites and cancer.
Testosterone Trials
The Testosterone Trials were a coordinated set of seven placebo-controlled, double-blind trials in 788 men with a mean age of 72 years to determine the efficacy of increasing the testosterone levels of older men with low testosterone.
Researchers found that testosterone treatments improved bone density and anemia, but did not improve patients' cognitive function, and it increased the amount of plaque buildup in the participants' coronary arteries.
Hemophilia
Researchers led the MyLifeOurFuture program, created in 2017, which has genotyped over 11,000 individuals with hemophilia across the U.S.
Prostate Cancer Genetics Research
Researchers identified germline mutations – BRCA1, BRCA2 and others, including some that are also connected with inherited breast and ovarian cancers – in men with metastatic prostate cancer, prompting the National Comprehensive Cancer Network to update its prostate cancer guidelines in 2019 to recommend genetic testing.
Undiagnosed Diseases
In 2018, the University of Washington joined the National Undiagnosed Diseases Network, which brings together clinical and research experts from across the United States to solve the most challenging medical mysteries using advanced technologies.
Paving the way
 Dr. Bessie Young became the first African American female professor in the Department of Medicine in 2015. A health disparities and inequities researcher, she works to identify and improve outcomes for marginalized communities. In 2010, the Young Endowed Scholarship was created to help underrepresented and marginalized medical students.
Dr. Bessie Young became the first African American female professor in the Department of Medicine in 2015. A health disparities and inequities researcher, she works to identify and improve outcomes for marginalized communities. In 2010, the Young Endowed Scholarship was created to help underrepresented and marginalized medical students.
She currently serves as medical director and vice dean for healthcare equity for UW Medicine and the School of Medicine.
Visiting Scholars Program
The Visiting Scholars Program welcomed its first student in 2015. This is a funded program designed to give medical students with diverse backgrounds a chance to experience the training that the Department of Medicine has to offer.
Wearable artificial kidney
 In 2015, the U.S. Food and Drug Administration fast-tracked the Wearable Artificial Kidney – one of the first innovations in dialysis technology in decades – after it performed successfully in its first U.S. clinical trial at the University of Washington Medical Center.
In 2015, the U.S. Food and Drug Administration fast-tracked the Wearable Artificial Kidney – one of the first innovations in dialysis technology in decades – after it performed successfully in its first U.S. clinical trial at the University of Washington Medical Center.
Mini-organs
 In 2015, researchers successfully grew mini-kidney organoids from pluripotent stem cells. They then used a gene-editing technique to engineer the organoids with genetic changes linked to kidney disease, re-creating kidney disease in a petri dish and paving the way for personalized kidney regeneration and drug testing.
In 2015, researchers successfully grew mini-kidney organoids from pluripotent stem cells. They then used a gene-editing technique to engineer the organoids with genetic changes linked to kidney disease, re-creating kidney disease in a petri dish and paving the way for personalized kidney regeneration and drug testing.
In 2018, an automated system was developed that uses robots to rapidly produce human mini-organs derived from stem cells, expanding the use of mini-organs in basic research and drug discovery.
Genetics and inherited cancers

Dr. Mary-Claire King discovered the first gene responsible for inherited breast and ovarian cancer, changing the prevention and treatment of these diseases.
Also, beginning in the 1980s, working with the Grandmothers of the Plaza de Mayo, she developed familial genetic matching to uncover and resolve human rights abuses, first in Argentina and then worldwide.
In 2016, she was presented with the National Medal of Science by President Obama, who said, “Every single American should be grateful for Mary-Claire King’s path.”
Blood pressure and genetics
Researchers found over 1000 genetic signals that influence blood pressure, which allows a way to calculate a person’s genetic risk score for high blood pressure late in life and target early interventions to those at high genetic risk.
Male hormonal contraceptives

For the last five decades, researchers have led work aimed at developing effective, reversible male hormonal contraceptives.
In 2010, the University of Washington became one of two sites selected to lead the National Institutes of Health-funded Male Contraceptive Clinical Trials Network.
Promising results of a prototype male contraceptive pill were presented in 2018 and in 2019, the first efficacy study of a self-administered male hormonal contraceptive was launched.
The study, currently underway at 17 sites across the globe, is also the first male contraceptive efficacy study to include sites in Africa.
This study could lead to the approval of the first reversible, novel male contraceptive to reach the market in over 300 years (the last one being the condom).
Hepatitis C
In 2016, researchers found that 12-week treatments can cure most hepatitis C patients, paving the way to potentially curing almost all U.S. veterans in its care who have hepatitis C. Since then, the VA has cured over 100,000 veterans with chronic hepatitis C.
In 2018, the UW Medicine Heart Transplant Program successfully cured the first hepatitis C-negative recipient of a hepatitis C-positive donor heart.
Merkel cell carcinoma
Research from two pivotal clinical trials showed immunotherapy drugs have long-term benefits for patients with Merkel cell carcinoma, a deadly skin cancer, changing the standard of care and gaining drug approval from the U.S. Food and Drug Administration, the cancer’s first.
Psoriasis and psoriatic arthritis
Researchers played a key role in the development of anti-IL-17 receptor A (brodalumab), approved in the U.S. and Europe for the treatment of psoriasis and psoriatic arthritis in 2017.
A partnership to train physician scientists
The joint University of Washington-Morehouse School of Medicine Medical Scientist Training Program was formed and the first student started in 2016.
Visiting Resident Scholars Program
Created as a result of the highly successful Visiting Scholars Program for medical students, the Visiting Resident Scholars Program was created in 2019.
 Diabetes Institute
Diabetes Institute
The UW Medicine Diabetes Institute, the first of its kind in the Pacific Northwest, was founded in 2019, creating a “bench to bedside” institute dedicated to advancing the understanding and treatment of diabetes and its complications.

Jung becomes department chair
In 2019, Dr. Barbara Jung became the sixth chair of the Department of Medicine, after serving as division chief of Gastroenterology and Hepatology at the University of Illinois Chicago.
Centers founded
- Cambia Palliative Care Center of Excellence
- Center for Cardiovascular Innovation
- Center for Dialysis Innovation
- Center for Emerging & Re-Emerging Infectious Diseases
- Center for Innate Immunity and Immune Disease
- Center for Liver Investigation Fostering Discovery
- Center for Patient Care Quality and Safety
- Center for Progress in Resuscitation
- Diabetes Institute
- Firland Northwest Tuberculosis Center
- Kenya Research and Training Center
- Microbial Interactions & Microbiome Center
(Originally the Center for Microbiome Sciences & Therapeutics) - Pacific NW Undiagnosed Diseases Network
- Tuberculosis Research and Training Center
2020s

Latinx Diabetes Institute

The Latinx Diabetes Clinic opened in 2020 to decrease healthcare disparities in Latinx patients with diabetes and address cultural and linguistic barriers to high-quality care for this underserved population.
The largest and fastest-growing minority group in the state of Washington and the country, Latinx individuals are disproportionately affected by diabetes.
Genetic Counseling Graduate Program
The inaugural genetic counseling graduate program – the only degree-awarding program in the Department of Medicine – enrolled its first class of 14 students in 2021.
Artificial intelligence to monitor heart rhythms
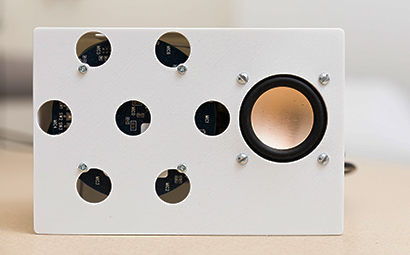 The first artificial intelligence system to monitor heart rhythms was developed in 2021, allowing, for the first time, smart speakers to monitor regular and irregular heartbeats without physical contact.
The first artificial intelligence system to monitor heart rhythms was developed in 2021, allowing, for the first time, smart speakers to monitor regular and irregular heartbeats without physical contact.
AI and nanotechnology
Researchers discovered a technique that combines nanotechnology with artificial intelligence to diagnose tuberculosis in children, in whom the deadly disease might otherwise go undetected.
Global Cardiovascular Health
 Cardiovascular disease remains the leading cause of death across the globe. The landmark Global Burden of Disease study – now in its third decade – quantifies health loss from hundreds of diseases, injuries, and risk factors, so that health systems can be improved and disparities eliminated.
Cardiovascular disease remains the leading cause of death across the globe. The landmark Global Burden of Disease study – now in its third decade – quantifies health loss from hundreds of diseases, injuries, and risk factors, so that health systems can be improved and disparities eliminated.
The Global Cardiovascular Health Program was established in 2021, dedicated to global cardiovascular disease prevention and care.
Pulmonary regurgitation
In 2021, Cardiologists became the first in Washington state to offer a new catheter-placed valve for patients with severe pulmonary regurgitation.
Cognition in Primary Care Program
The Cognition in Primary Care Program was launched in 2021 to train primary care providers to facilitate detection of cognitive impairment and improve care for people with dementia.
 Outreach medicine
Outreach medicine
The Harborview Medical Center Mobile Health Outreach Program was established in 2021 to meet the needs of medically underserved community members.
Bionic Pancreas
In 2022, researchers found that a pocket-size wearable device known as a bionic pancreas – which uses next-generation technology to automatically deliver insulin – was more effective at maintaining blood glucose levels within normal range than standard-of-care management among people with type 1 diabetes.
Heart tumor repair
Cardiologists performed a first-in-human procedure, successfully employing a catheter-delivered device to retrieve a benign tumor from inside a patient’s heart in 2022.
Catheter-placed mitral valve
In 2023, Cardiologists performed a first-in-the-world procedure, detaching and retrieving a clip device from a patient’s mitral valve and placing a replacement biologic valve — all through a catheter. Previously this sequence of tasks had been performed only via open-heart surgery.

Harvey Alter receives Nobel Prize
Dr. Harvey Alter, a resident in the UW Internal Medicine Residency Program from 1964-1965, received the 2020 Nobel Prize in Medicine for his contributions to the discovery of the Hepatitis C virus.
Health Equity
In 2021, the Internal Medicine Residency Program's Health Equity Pathway was established to equip residents in applying anti-oppression frameworks to combat the structural origins of health inequities in clinical care and advocacy.
In 2022, recent graduates of the Internal Medicine Residency Program received a grant from leading internal medicine organizations to build a longitudinal Health Equity and Anti-Racism curriculum.
Removal of race modifiers from eGFR equations
In 2020, advocacy efforts among students, faculty, and staff led to the removal of the race coefficient from Estimated Glomerular Filtration Rate (eGFR) reporting from UW Medicine Laboratory testing, which subsequently led to national recognition and removal of race modifiers from eGFR equations in 2021 and 2022.
Alaska Residency Program
Established in 2023 and based in Soldotna, Alaska, the University of Washington-Alaska Internal Medicine Rural Residency Program is the very first accredited rural residency training program in internal medicine in the country.

Center for Indigenous Health
The Center for Indigenous Health was formed in 2023 to expand opportunities for American Indian and Alaska Native premedical students, medical students and academic faculty throughout the full spectrum of educational and career stages
Colorectal cancer screening
A novel pilot rideshare program – the first of its kind in the country – found that rideshare can be a viable solution to connect patients to colonoscopy procedures.
3-Wishes Project
 The 3-Wishes Project, brought to the University of Washington in 2023, is an end-of-life program that aims to improve the experience for patients, families, and healthcare team members by fulfilling wishes for dying patients and their loved ones.
The 3-Wishes Project, brought to the University of Washington in 2023, is an end-of-life program that aims to improve the experience for patients, families, and healthcare team members by fulfilling wishes for dying patients and their loved ones.
Portable artificial kidney
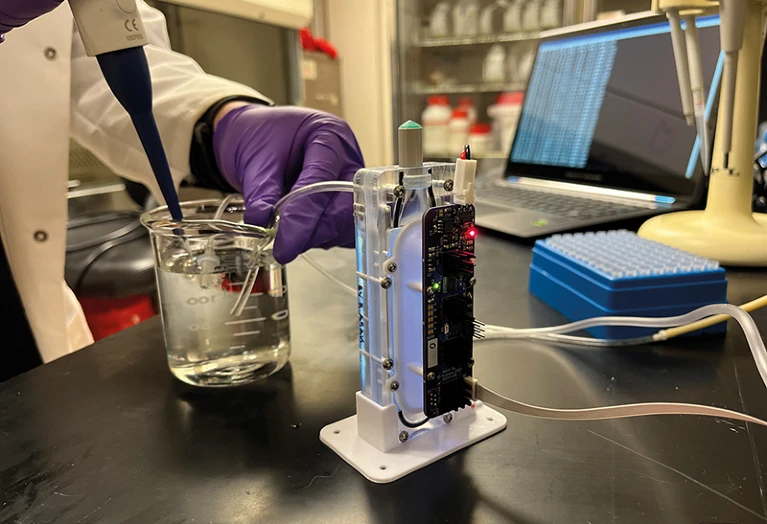 Researchers at the Center for Dialysis Innovation are currently developing an artificial kidney that recycles dialysate — the liquid that removes urea and adds back electrolytes — instead of using liters of water to flush it away.
Researchers at the Center for Dialysis Innovation are currently developing an artificial kidney that recycles dialysate — the liquid that removes urea and adds back electrolytes — instead of using liters of water to flush it away.
Pandemic response
Seattle Flu Study
The Seattle Flu Study – a first-of-its-kind citywide network for infectious disease – launched in 2018 to better understand how influenza and other contagious diseases spread, and to gather information about how they might be better detected, monitored and controlled.
In early January 2020, the Seattle Flu Study team pivoted to detect and understand the spread of SARS-CoV-2 throughout the Seattle area and became one of first research groups to conduct genome sequencing of the virus, which informed understanding of how COVID-19 was changing and spreading in the King County area.
Clinical trials
 Researchers designed and oversaw USG Operation Warp Speed Covid-19 Phase 3 vaccine trials, and the UW Vaccine and Treatment Evaluation Units were among the highest enrolling sites for the Phase 3 trial of the Novavax Covid-19 vaccine.
Researchers designed and oversaw USG Operation Warp Speed Covid-19 Phase 3 vaccine trials, and the UW Vaccine and Treatment Evaluation Units were among the highest enrolling sites for the Phase 3 trial of the Novavax Covid-19 vaccine.
Taking the lessons learned from the HIV epidemic, early in 2020 leading infectious disease experts developed a model for rapid development and clinical testing of vaccines.
The COVID-19 Prevention Network was established to coordinate massive trials of several vaccine candidates.
The COVID-19 Clinical Research Center opened in 2020, one of the first facilities in the nation designed to test novel interventions to treat and prevent COVID-19.
Outreach
COVID-19 vaccine research and studies of long COVID have been conducted in collaboration with the Lummi Nation and Nooksack Indian Tribe.
Researchers led a program to increase testing access for rural and underserved populations and launched a study of COVID-19 in Seattle’s homeless community.
A rapid, point-of-care test was developed for use in community-based or resource-limited settings.
Long COVID
Researchers are leading the RECOVER (Researching COVID to Enhance Recovery) study, which is the largest and most comprehensive long COVID research effort in the U.S. to date.
Investigators found that SARS-CoV-2 causes inflammation in the brain, adding a major piece to the puzzle of how a lung disease becomes long COVID, a disease of the brain.
A multidisciplinary study was funded in 2023 to expand and improve access to care for people with long COVID, particularly underserved, rural, vulnerable and minority populations that were disproportionately impacted.
Healing the healers
One in five healthcare workers around the world has suffered from anxiety and/or depression during the pandemic.
For the first time, researchers at the University of Washington are using frontline healthcare workers as patients to examine the effect of psilocybin – the psychoactive ingredient in “magic mushrooms” – on treating depression.
 United World for Antiviral Research Network
United World for Antiviral Research Network
The University of Washington is part of the United World for Antiviral Research Network, formed in 2020 to provide surveillance for emerging pandemic viruses, develop urgently needed diagnostics and therapeutics, and expand understanding of viral immune responses, which is key to vaccine development.
Lupus
Researchers led the development of anti-interferon receptor 1 (anifrolumab), approved by the FDA for the treatment of lupus in 2021.
Investigators demonstrated the previously not understood mechanism in which UV light exposure in lupus patients leads to local inflammation of the skin and systemic inflammation of other organs including the kidneys.
Cervical cancer
A research trial in 2021 showed that a single dose efficacy was the same as multiple doses of the human papillomavirus (HPV) vaccine, which could hasten the pace of vaccination and bring renewed energy to the push to make cervical cancer the first cancer to be wiped out globally.
Breast cancer
An experimental vaccine against breast cancer safely generated a strong immune response to a key tumor protein, leading us closer to a vaccine that can effectively treat patients with breast cancer.
Data from the University of Washington was critical in garnering FDA approval for the first PET imaging agent for breast cancer patients in 2022.
Immunotherapy
In 2023, physicians successfully used CAR T-cell therapy to treat a patient with post-transplant lymphoproliferative disorder, only the 17th patient in the world to receive this life-saving therapy.
Immunotherapy has recently been successful in patients with advanced chondrosarcoma, a cancer of the cartilage.
Early clinical trials will test CAR T cells against advanced prostate cancer.
Metastatic urothelial carcinoma
Multi-institutional trials led to the FDA approval of avelumab and sacituzumab for treatment of metastatic urothelial carcinoma.
Financial hardship for cancer patients
The risk of adverse financial events in patients with cancer was evaluated through a novel linkage between cancer registry and credit records.
Genomics
Genomic study on stroke
Results from the largest genomic study on stroke showed preliminary insights into the specific genes involved and the biological mechanisms through which they may contribute to the occurrence of stroke, informing drug discovery and risk prediction across ancestries.
Genomic risk assessment
The Electronic Medical Records and Genomics (eMERGE) Genomic Risk Assessment and Management Network was established in 2020 to establish protocols and methodologies for improved genomic risk scoring for diverse populations.
Advances in transplant care
Living donors
In 2020, a UW Medicine team performed a first-in-Pacific Northwest living-donor liver transplant for metastatic colorectal cancer.
The Cancer and Organ Transplant Clinic opened in 2021, a first-of-its-kind multidisciplinary consult clinic that combines transplant and oncology expertise.
The Living Donor Liver Transplant Program had the highest volume of adult to pediatric liver transplants in the U.S. in 2022 and is the only group in the Pacific Northwest performing liver transplants in this innovative manner.
Donation-after-circulatory-death
LifeCenter Northwest and UW Medicine facilitated the Pacific Northwest’s first donation-after-circulatory-death heart transplant in 2022.
Transplant Institute
Launched in 2022 and co-led by Department Chair Barbara Jung, the UW Medicine Transplant Institute brings together UW Medicine’s organ transplant services: liver, kidney, pancreas, and lung.

Dual organ transplant
In a historic procedure in 2023, a patient received two donor organs, a liver and a heart, to prevent the extremely high likelihood that her body would reject a donor heart transplanted alone.
Growth hormone replacement therapy for brain injuries
Researchers in a multicenter study being implemented in 20 VA Centers across the United States are testing the safety and efficacy of growth hormone replacement therapy to improve the quality of life of Veterans with traumatic brain injuries.
Portable screening test for neurological disorders
Researchers have developed Beacon: a novel, portable device that measures critical flicker frequency (a screening test for hepatic encephalopathy, a neurological disorder impacted by chronic liver disease) through a smartphone app, making testing more accessible.
Advances in dementia research
Atrial fibrillation and dementia
Researchers found that people with a recent diagnosis of atrial fibrillation, the most common irregular heart rhythm, have a 13% higher risk of developing dementia than people without the condition.
Targeting tau and its impact on dementia diseases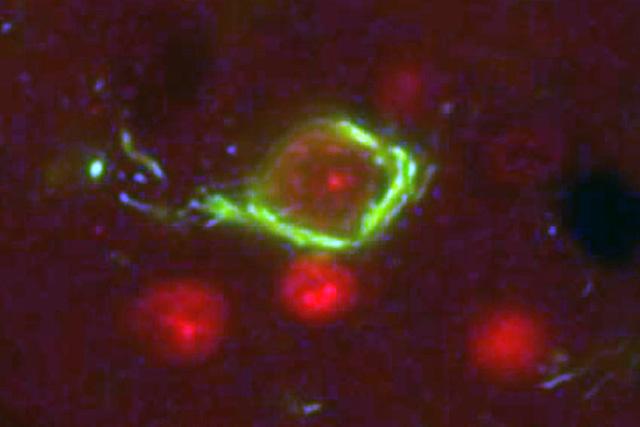
In 2022, the drug lacanemab was reported to slow the progression of Alzheimer’s disease, the first time a drug was able to affect the course of this disease.
Lacanemab targets beta-amyloid, and University of Washington researchers are focusing on targeting the protein tau, which is most closely tied to the decline in cognitive dysfunction.
Breakthrough in STI prevention
 A common antibiotic, doxycycline, is poised to become a “morning-after” pill to reduce the spread of chlamydia, syphilis and gonorrhea among populations at higher risk for contracting those bacterial infections.
A common antibiotic, doxycycline, is poised to become a “morning-after” pill to reduce the spread of chlamydia, syphilis and gonorrhea among populations at higher risk for contracting those bacterial infections.
UW researchers led one of the studies whose findings led to the Centers for Disease Control (CDC) recommendation of “doxy-PEP” (doxycycline post-exposure prophylaxis).
Looking to the future
The Department of Medicine has been at the forefront of innovation in healthcare since 1948, and we look forward to building on our past successes, embracing new opportunities, and tackling the challenges of tomorrow.
As the academic leader in the region, we will continue to focus on delivering culturally sensitive care and understanding and representing the populations we are
treating, training the future leaders of medicine, and performing transformative medical research resulting in groundbreaking, patient-centered scientific discovery.